Artificial Disc
Perhaps the most anticipated advance in spine surgery over the past 30 years was the arrival of the artificial disc. The first artificial disc in the United States received formal approval by the Food and Drug Administration (FDA) for widespread use in the United States on October 26, 2004.

Long before that, artificial disc replacement has been used in Europe and other advanced countries as an alternative to spinal fusion for motion preservation. Because of the FDA — which regulates the approval of new technology in the United States — new medical technology must go through rigorous clinical studies to prove efficacy and value over existing treatment options.
The traditional treatment used for herniated discs over the last 40 years has been spinal fusion, which replaces the damaged disc with a piece of bone (from the patient’s hip for from a bone bank) that is inserted in the disc space between the two vertebrae. This locks the vertebrae together, preventing movement.
Research studies from the North American Spine Society, however, have documented that spinal fusion, which locks two vertebrae together, can cause other discs to herniate above and below the fusion level. This is called “adjacent segment disease.”

Artificial disc replacement is viewed to be like artificial hip replacement or artificial knee replacement. At the early part of the century, the traditional treatment for arthritic knees and hips was to fuse and lock the joint. That is now unthinkable considering that joint replacement is now commonplace and done in outpatient surgery. The same can be said for artificial disc replacement in the neck.
Those surgeons who are proficient in artificial disc replacement in the neck can perform the surgery and have patients home the same day.
 Insurance companies in the United States are often reluctant to cover new technology and that was somewhat the case up to 2020. However that reluctance is now fading as artificial disc replacement is becoming that new standard of care — especially for herniated discs in the neck.
Insurance companies in the United States are often reluctant to cover new technology and that was somewhat the case up to 2020. However that reluctance is now fading as artificial disc replacement is becoming that new standard of care — especially for herniated discs in the neck.
It is important to remember that this technology is still evolving with new implants continually in development. Dr. Rory Mayer can discuss if it is appropriate for you, and what model of artificial disc is best suited for your case.
Artificial Disc Replacement with Dr. Rory Mayer in Austin, Texas
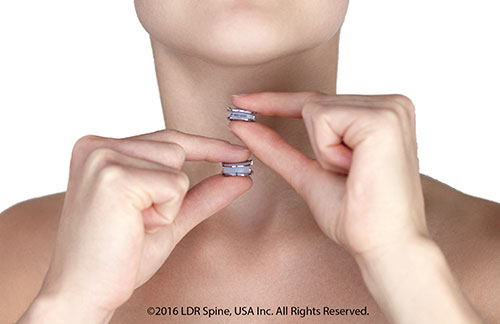 It’s estimated that over 1 million people in the United States have neck pain related to cervical disc herniations. Consequently, each year in the United States about 266,000 neck surgeries are performed to relieve symptoms of weakness, numbness or radiating pain into an arm or hand. It’s estimated that more than 10% of these neck surgeries involved the use of an artificial disc, with the percent growing rapidly each year. That’s because more insurance companies are recognizing the value of artificial disc surgery over traditional fusion surgery which locks two vertebrae together, causing less rotation of the neck and future problems with other disc levels. Research from the North American Spine Society has documented that the preferred treatment for disc herniations in the neck is now artificial disc replacement.
It’s estimated that over 1 million people in the United States have neck pain related to cervical disc herniations. Consequently, each year in the United States about 266,000 neck surgeries are performed to relieve symptoms of weakness, numbness or radiating pain into an arm or hand. It’s estimated that more than 10% of these neck surgeries involved the use of an artificial disc, with the percent growing rapidly each year. That’s because more insurance companies are recognizing the value of artificial disc surgery over traditional fusion surgery which locks two vertebrae together, causing less rotation of the neck and future problems with other disc levels. Research from the North American Spine Society has documented that the preferred treatment for disc herniations in the neck is now artificial disc replacement.
Dr. Rory Mayer uses three FDA-approved artificial discs to replace disc herniations in the neck:
- Mobi-C artificial disc
- Simplify artificial disc
- M6 artificial disc
Dr. Mayer evaluates a person’s disc herniation to determine which disc would be a better fit for the patient.
 Mobi-C was the first disc approved by the FDA for two levels in the neck. Accordingly over the years, the Mobi-C disc is one of the most widely used cervical discs in the world. According to the manufacturer, Mobi-C has been implanted more than 17,000 time across 25 countries. According to one study, patients receiving the Mobi-C disc returned to work and activity 3 weeks earlier than those with traditional fusion surgery. Mobi-C contains a polyethylene core that slides and rotate inside the disc for self-adjustment to the cervical spine movements. This means that Mobi-C can react to the normal motion in the cervical spine. Mobi-C provides bone sparing fixation without chisel cuts into the small vertebral bodies of the cervical spine, making it a safer option when used at two levels.
Mobi-C was the first disc approved by the FDA for two levels in the neck. Accordingly over the years, the Mobi-C disc is one of the most widely used cervical discs in the world. According to the manufacturer, Mobi-C has been implanted more than 17,000 time across 25 countries. According to one study, patients receiving the Mobi-C disc returned to work and activity 3 weeks earlier than those with traditional fusion surgery. Mobi-C contains a polyethylene core that slides and rotate inside the disc for self-adjustment to the cervical spine movements. This means that Mobi-C can react to the normal motion in the cervical spine. Mobi-C provides bone sparing fixation without chisel cuts into the small vertebral bodies of the cervical spine, making it a safer option when used at two levels.
Simplify is one of the latest artificial disc designs and has become popular with many spine surgeons. Drl Mayer notes that the Simplify Disc is somewhat unique in that it is fully viewable on MRI after surgery is completed. This minimizes a patient’s exposure to radiation from CT scans which would otherwise have to be used. Proponents say that because the Simplify disc doesn’t metal in its articulating components, it may be undergo less wear over time that may occur in other designs. Also surgery to install the Simplify disc is somewhat easier than other artificial discs for the neck. Lastly, the Simplify disc comes in different sizes for patients of different body size. The Simplify disc comes in a variety of heights from 4mm, 5mm and 6mm. The smaller 4mm disc height makes it ideal for female patients or small patients with smaller cervical disc spaces. Some surgeons believe the Simplify disc better mimics the natural motion of the neck for ideal motion preservation.
About the M6 artificial disc in the neck
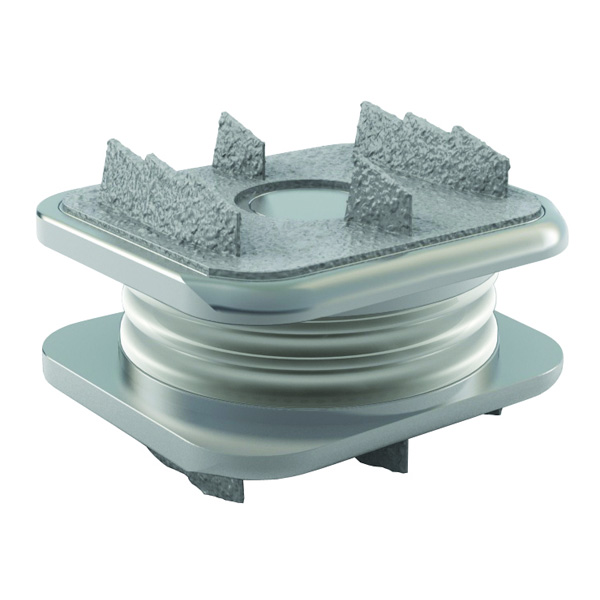 Dr. Rory Mayer also uses the M6 artificial disc in the neck for patients who desire to preserve motion preservation and avoid an ACDF spinal fusion. The key difference of the M6 artificial disc is that the design provides some up/down shock absorption in addition to rotation.
Dr. Rory Mayer also uses the M6 artificial disc in the neck for patients who desire to preserve motion preservation and avoid an ACDF spinal fusion. The key difference of the M6 artificial disc is that the design provides some up/down shock absorption in addition to rotation.
A clinical study related to the M6 disc involving 160 patients who received the M6 disc, found M6-C patients had a notable reduction of pain and need for opiod drugs for pain relief use after surgery compared to 189 ACDF patients. At 24 months, patients in the ACDF group who were still using pain medications had a seven times higher rate of opioid use than those in the M6- C disc group. Prior to surgery, 80.6% of the M6-C disc patients and 85.7% of the ACDF patients were taking some type of pain medication for pain symptoms related to their herniated disc in the neck.
Patients who received the M6-C disc also had significant improvement in function as measured with the Neck Disability Index. Patients receiving the M6-C disc also reported a 92% satisfaction rate with the surgery, with 93% said they would have the surgery again.
 The surgery time involved was also shorter for implantation of the M6 artificial disc compared to spinal fusion (ACDF). Mean surgery time was 74 minutes for M6 patients compared to two hours in the operating room for those patients having the ACDF procedure. Hospital stay was also shorter for M6 patients with most going home the same day while fusion patients had a one day hospital stay. Subsequent surgery for the disc level was only needed in 1.9% of the M6-C disc patients compared to 4.8% of the ACDF patients.
The surgery time involved was also shorter for implantation of the M6 artificial disc compared to spinal fusion (ACDF). Mean surgery time was 74 minutes for M6 patients compared to two hours in the operating room for those patients having the ACDF procedure. Hospital stay was also shorter for M6 patients with most going home the same day while fusion patients had a one day hospital stay. Subsequent surgery for the disc level was only needed in 1.9% of the M6-C disc patients compared to 4.8% of the ACDF patients.
The M6 artificial disc is comprised of ultra-high molecular weight polyethylene fiber wound around a polycarbonate urethane polymer core. The design is intended to mimic a natural disc by providing some shock absorption as well as a controlled range of motion. By preserving more natural movement of the neck, the M6-C disc minimizes the stress on spinal discs above and below the herniated disc level.
Artificial disc replacement in the low back:
Currently, Dr. Mayer does not do LUMBAR disc replacements because the artificial disc technology for the low back is evolving and changing rapidly. Also the lumbar discs have more load placed on the disc from the bodyweight of the patient.
Dr. Rory Mayer is a fellowship-trained spine surgeon based in Austin, Texas with Texas Spine and Scoliosis, which is a regional spine center of excellence. This multi-disciplinary spine center combines the expertise of fellowship-trained orthopedic and neurosurgical spine surgeons; physical medicine doctors who provide non-surgical treatment options for back pain and neck pain including spinal injections; and spine specialized physical therapists — all under one roof. The regional spine center is referred patients from across Central Texas, including Austin, San Antonio, Houston, East Texas and West Texas. International patients from cities across Mexico — including Mexico City, Monterrey, Hermosillo and Merida — come to the spine center for second opinions for spine surgery and treatment for scoliosis (curvature of the spine); spinal tumor and artificial disc replacement. Dr. Mayer in particular specializes in adult scoliosis, treatment and correction of flatback syndrome, removal of spinal tumor, minimally invasive spine surgery and artificial disc replacement surgery.
